Pelvic Congestion Syndrome Natural Treatment and Causes
How to Read Your Body
Learn to recognize common symptoms and uncover their underlying health issues
Understand the signs of nutrient deficiencies to manage your health
Explore the four metabolic body types and the core factors that influence them
Interpret your body's signals from head to toe to identify potential health concerns
How to Read Your Body
Learn to recognize common symptoms and uncover their underlying health issues
Understand the signs of nutrient deficiencies to manage your health
Explore the four metabolic body types and the core factors that influence them
Interpret your body's signals from head to toe to identify potential health concerns
How to Read Your Body
Learn to recognize common symptoms and uncover their underlying health issues
Understand the signs of nutrient deficiencies to manage your health
Explore the four metabolic body types and the core factors that influence them
Interpret your body's signals from head to toe to identify potential health concerns
How to Read Your Body
Learn to recognize common symptoms and uncover their underlying health issues
Understand the signs of nutrient deficiencies to manage your health
Explore the four metabolic body types and the core factors that influence them
Interpret your body's signals from head to toe to identify potential health concerns
How to Read Your Body
Learn to recognize common symptoms and uncover their underlying health issues
Understand the signs of nutrient deficiencies to manage your health
Explore the four metabolic body types and the core factors that influence them
Interpret your body's signals from head to toe to identify potential health concerns
How to Read Your Body
Learn to recognize common symptoms and uncover their underlying health issues
Understand the signs of nutrient deficiencies to manage your health
Explore the four metabolic body types and the core factors that influence them
Interpret your body's signals from head to toe to identify potential health concerns
How to Read Your Body
Learn to recognize common symptoms and uncover their underlying health issues
Understand the signs of nutrient deficiencies to manage your health
Explore the four metabolic body types and the core factors that influence them
Interpret your body's signals from head to toe to identify potential health concerns
How to Read Your Body
Learn to recognize common symptoms and uncover their underlying health issues
Understand the signs of nutrient deficiencies to manage your health
Explore the four metabolic body types and the core factors that influence them
Interpret your body's signals from head to toe to identify potential health concerns
How to Read Your Body
Learn to recognize common symptoms and uncover their underlying health issues
Understand the signs of nutrient deficiencies to manage your health
Explore the four metabolic body types and the core factors that influence them
Interpret your body's signals from head to toe to identify potential health concerns
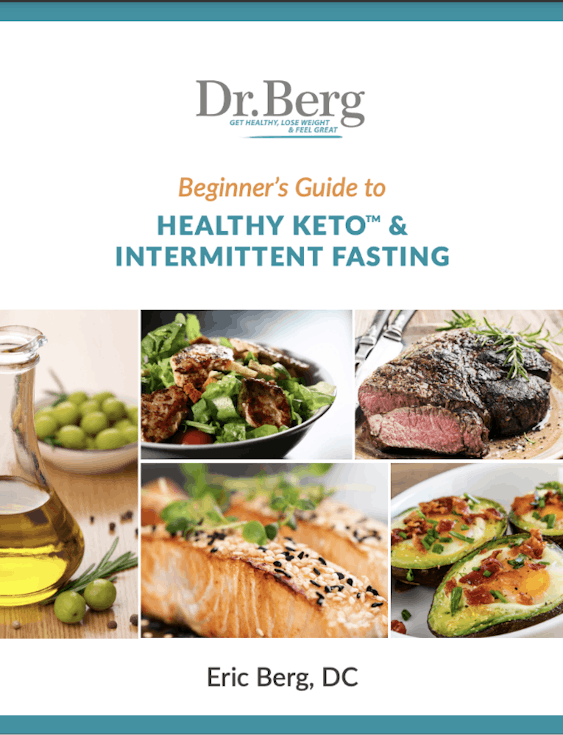
Beginner’s Guide to Healthy Keto & Intermittent Fasting
Receive a step-by-step guide to starting Healthy Keto® and intermittent fasting
Learn about foundational principles and best practices for beginners
Get detailed visual guidance on portion sizes and meal composition
Discover how to set achievable goals and monitor your progress
Find practical tips for overcoming common challenges and staying motivated
Beginner’s Guide to Healthy Keto & Intermittent Fasting
Receive a step-by-step guide to starting Healthy Keto® and intermittent fasting
Learn about foundational principles and best practices for beginners
Get detailed visual guidance on portion sizes and meal composition
Discover how to set achievable goals and monitor your progress
Find practical tips for overcoming common challenges and staying motivated
Beginner’s Guide to Healthy Keto & Intermittent Fasting
Receive a step-by-step guide to starting Healthy Keto® and intermittent fasting
Learn about foundational principles and best practices for beginners
Get detailed visual guidance on portion sizes and meal composition
Discover how to set achievable goals and monitor your progress
Find practical tips for overcoming common challenges and staying motivated
Beginner’s Guide to Healthy Keto & Intermittent Fasting
Receive a step-by-step guide to starting Healthy Keto® and intermittent fasting
Learn about foundational principles and best practices for beginners
Get detailed visual guidance on portion sizes and meal composition
Discover how to set achievable goals and monitor your progress
Find practical tips for overcoming common challenges and staying motivated
Beginner’s Guide to Healthy Keto & Intermittent Fasting
Receive a step-by-step guide to starting Healthy Keto® and intermittent fasting
Learn about foundational principles and best practices for beginners
Get detailed visual guidance on portion sizes and meal composition
Discover how to set achievable goals and monitor your progress
Find practical tips for overcoming common challenges and staying motivated
Beginner’s Guide to Healthy Keto & Intermittent Fasting
Receive a step-by-step guide to starting Healthy Keto® and intermittent fasting
Learn about foundational principles and best practices for beginners
Get detailed visual guidance on portion sizes and meal composition
Discover how to set achievable goals and monitor your progress
Find practical tips for overcoming common challenges and staying motivated
Beginner’s Guide to Healthy Keto & Intermittent Fasting
Receive a step-by-step guide to starting Healthy Keto® and intermittent fasting
Learn about foundational principles and best practices for beginners
Get detailed visual guidance on portion sizes and meal composition
Discover how to set achievable goals and monitor your progress
Find practical tips for overcoming common challenges and staying motivated
Beginner’s Guide to Healthy Keto & Intermittent Fasting
Receive a step-by-step guide to starting Healthy Keto® and intermittent fasting
Learn about foundational principles and best practices for beginners
Get detailed visual guidance on portion sizes and meal composition
Discover how to set achievable goals and monitor your progress
Find practical tips for overcoming common challenges and staying motivated
Beginner’s Guide to Healthy Keto & Intermittent Fasting
Receive a step-by-step guide to starting Healthy Keto® and intermittent fasting
Learn about foundational principles and best practices for beginners
Get detailed visual guidance on portion sizes and meal composition
Discover how to set achievable goals and monitor your progress
Find practical tips for overcoming common challenges and staying motivated
Pelvic congestion syndrome (PCS) is a medical condition characterized by chronic pain in the pelvic region. PCS occurs due to the development of varicose veins in the lower abdomen that restrict normal blood flow, resulting in pain and discomfort.
PCS is more common in women and can be caused by various factors, including hormonal changes, pregnancy, and genetic predisposition.
Let’s look at common causes of PCS and what steps you can take to ease symptoms fast.

What is pelvic congestion syndrome (PCS)?
Blood vessels in the lower abdomen can become varicose, resulting in twisted and enlarged veins that no longer function properly.
Varicose pelvic veins can’t drain blood effectively from the pelvic region. This increases pressure within the abdomen, resulting in discomfort and chronic pain, and can impede the ability to perform everyday activities, including exercising, walking, and lifting heavy objects.
Although more common in women, men also can suffer from PCS and typically develop varicose veins in the testicular area of the pelvis.
Signs of PCS
While most people with PCS suffer dull abdominal pain and increased pressure in the pelvic region, it can cause a wide range of other symptoms.
These are common pelvic congestion syndrome symptoms:
Chronic pelvic pain
Dull or aching pain that may be worse on one side of the pelvis
A feeling of fullness or pressure in the pelvic area
Pain during intercourse
Lower back pain
Pain worsens after long periods of standing or sitting
Abdominal bloating or swelling
Dysmenorrhea or painful periods

Causes of PCS
PCS develops as a result of varicose pelvic veins, and it's thought that several potential causes can contribute to the formation of twisted and engorged blood vessels.
Hormonal changes
Hormonal fluctuations during the menstrual cycle, pregnancy, and menopause can cause the pelvic veins to dilate and lose muscle tone.
Women with multiple pregnancies are more likely to develop PCS. It's thought that high estrogen levels during pregnancy can cause thinning of vein walls, significantly increasing the risk of varicose pelvic veins.
Genetic predisposition
Research suggests that some people may have a genetic predisposition to developing PCS.
Obesity
Obesity can increase the risk of developing PCS. It's thought that excessive body weight increases pelvic pressure, which can result in enlarged pelvic veins.
Pelvic inflammation
Conditions including endometriosis, ovarian cysts, pelvic inflammatory disease, and pelvic infections can cause veins to become inflamed, which is linked to loss of vein elasticity and blood vessel wall thinning.
Pelvic surgery
Procedures such as hysterectomy or prostate removal can cause damage to pelvic veins and increase the risk of PCS.
Stress
Research suggests that stress can cause muscle tension, which increases pressure on pelvic veins linked to pain and discomfort.
How is PCS diagnosed?
PCS can be difficult to diagnose because it’s characterized by symptoms similar to those of other conditions, including endometriosis and irritable bowel syndrome (IBS).
Some of the diagnostic procedures to confirm PCS are:
Physical exam
Pelvic ultrasound
Magnetic resonance imaging (MRI)
Laparoscopy
Depending on the underlying cause, there are several treatment options, including hormonal therapy, surgery, and ovarian vein embolization, a minimally invasive procedure that appears to relieve pain in many women with PCS successfully.

Lifestyle choices that may help PCS
If you have PCS, it's best to consult your doctor to explore the most appropriate treatment plan. However, some dietary and lifestyle habits can help you relieve pelvic pain.
Diet
Excessive weight can significantly impact pelvic health and increase the risk of PCS.
A balanced ketogenic diet focuses on nutrient-dense foods that promote the utilization of stored body fat as an energy source. A Healthy Keto® diet helps lose weight, promotes healthy nutrition, and supports strong blood vessels.
In addition, Healthy Keto includes plenty of fiber-rich foods that keep bowel movements regular and avoid constipation which has been found to alleviate pelvic discomfort in PCS patients.
Exercise
Exercise helps maintain a healthy body weight and can minimize blood accumulation in pelvic veins. Activities such as brisk walking or swimming have been found to improve pelvic circulation and ease pelvic pressure.
Avoid long periods of standing or sitting
Prolonged standing or sitting can increase the pressure on pelvic veins and cause fluid accumulation, worsening PCS symptoms.
Supplements
Research suggests that many botanical herbs and medicinal plants, including horse chestnut, grape seed blue cohosh, gotu kola, and red raspberry leaf, support the vascular tone of pelvic blood vessels and promote pelvic health.
Horse chestnut has been traditionally used to treat varicose veins. It contains aescin, a plant compound believed to help strengthen the walls of blood vessels and improve circulation. Some studies have suggested that horse chestnuts may effectively reduce PCS symptoms.
Red raspberry leaf tea may support pelvic health by promoting uterine blood flow and pelvic muscle tone, which may help ease PCS symptoms.

Key takeaways
Pelvic congestion syndrome results from enlarged and bulging pelvic veins that can’t adequately drain blood from the pelvic region, resulting in pelvic pressure, pain, and discomfort.
How your doctor will treat PCS will depend on the underlying cause. However, maintaining a healthy body weight, engaging in daily exercises—including walking or swimming—and avoiding long periods of standing or sitting supports your pelvic health and can ease PCS symptoms.
FAQ
1. What is PCS (pelvic congestion syndrome)?
Pelvic congestion syndrome is a condition in which pelvic veins become varicose. Varicose pelvic veins are enlarged and twisted and can’t properly drain blood away from the pelvic region, which causes pain, swelling, and abdominal discomfort.
2. What causes PCS?
Multiple pregnancies, obesity, and pelvic surgery can cause increased pelvic pressure that causes the thinning of pelvic blood vessel walls.
In addition, hormonal changes and genetic predisposition can contribute to the development of varicose pelvic veins and increase the risk of developing PCS.
3. How do you get rid of pelvic congestion?
The most appropriate treatment option will depend on the exact underlying cause and may include medications like birth control pills, surgery, or ovarian vein embolization.
4. Is pelvic congestion curable?
There isn’t a cure for pelvic congestion. However, a combination of medication, surgery, and the right lifestyle choices can help to manage PCS symptoms.
5. How can I reduce inflammation in my pelvic area?
A diet rich in anti-inflammatory nutrients can support your body to combat pelvic inflammation.
An anti-inflammatory diet avoids junk foods, sugar, and refined carbs and focuses on healthy fats such as olive oil and fish oils, nutrient-dense vegetables, organic dairy, and high-quality meats.
6. What supplements help pelvic pain?
Several supplements have been shown to promote pelvic health and support the functioning of pelvic veins, including grape seed, horse chestnut, blue cohosh, gotu kola, and red raspberry leaf extract.
7. Can stress make pelvic congestion syndrome worse?
Yes, stress can worsen symptoms of pelvic congestion syndrome.
8. What are the best natural remedies for PCS?
Natural treatments for PCS include herbal medicines, including horse chestnut and raspberry leaf tea to support pelvic health, gentle exercises to promote pelvic blood flow, and hydrotherapy to ease PCS symptoms and inflammation.
Previous blog
Ginger Shots: Health Benefits and Easy RecipeNext blog
Acetic Acid: Food Sources and BenefitsTags
Popular
08/21/2024
47K views
05/22/2024
41.2K views
11/18/2024
244.3K views
03/18/2024
11/21/2022




